Choose the Right Sports Medicine Expert
By
Christina Chapski, Ed.D., AT, ATC
Henry Ford Health
November 15, 2022
If you're an athlete, chances are you'll require specialized care from a health professional during your career.
 Confused about the differences between athletic trainers, sports medicine physicians and exercise physiologists, among other experts? You're not alone!
Confused about the differences between athletic trainers, sports medicine physicians and exercise physiologists, among other experts? You're not alone!
Each of these professionals has different levels of training, expertise and certifications, but the care they provide often overlaps. That's one reason why they often work together.
Sports Professionals Defined
Caring for athletes isn't always clear-cut. In fact, most athletes require a full team of professionals working in concert to stay at the top of their game. Yet confusion remains about which professionals you need to see for training, injury prevention, and recovery and treatment after an injury.
Each type of professional has its own set of experience, training and certifications. Here’s how they measure up:
· Sports medicine doctor: Sports medicine physicians are typically trained in orthopedic surgery, primary care or emergency medicine. These professionals have medical degrees as well as specialized training in sports medicine, including the prevention and treatment of injury. In addition to caring for conditions ranging from concussion to head colds, sports medicine physicians also focus on helping people return to sports safely and effectively after illness or injury.
· Athletic trainer: Athletic trainers take care of athletes from prevention through rehabilitation. In collaboration with a physician, these professionals offer insights that help minimize risk and prevent injuries. They evaluate athletes and provide immediate care and treatment, sometimes even on the sidelines. They also provide rehabilitation and reconditioning after an injury or illness.
· Exercise physiologist: Exercise physiologists study the effect of exercise on the muscular, cardiovascular, and sympathetic and parasympathetic nervous systems. They examine functional capacity and strength due to endurance training or strength training. These professionals may also test athletes for VO2max (your oxygen volume while training) and body composition (the ratio of fatty mass to lean mass).
· Physical medicine and rehab physician: These professionals treat a variety of medical conditions that affect the brain, spinal cord, nerves, bones, joints, ligaments, muscles and tendons. They take the whole body into account to pinpoint problems and enhance performance without surgery.
· Physical therapist: Physical therapists diagnose and treat individuals of all ages with conditions that limit their ability to move and perform daily activities.
Other Specialized Professionals Who Care for Athletes
In addition to the health care professionals described above, athletes may meet with a host of experts, including:
· Nurses and medical assistants
· Occupational therapists
· Cardiologists
· Neurologists
· Behavioral health specialists
· Dietitians
· Complementary medical practitioners, such as acupuncturists and chiropractors
None of these individuals are "fitness professionals," a term nearly anyone can use to describe a range of professional activities. Rather, these sports medicine experts are part of a comprehensive team that includes at least one physician. They are each licensed by the state to provide specialized care to athletes.
Personal trainers, on the other hand, focus on helping people find their way around the gym, hold them accountable to achieve their goals and help new exercisers and seasoned fitness enthusiasts stick to a workout regimen.
If you're an athlete, you need a team of health professionals who can provide comprehensive care to reach your highest potential.
Christina Chapski, Ed.D., AT, ATC, is the Director of Athletic Training & Community Outreach with Henry Ford Sports Medicine.
Want to learn more? Henry Ford Health System sports medicine experts are treating the whole athlete, in a whole new way. From nutrition to neurology, and from injury prevention to treatment of sports-related conditions, they can give your athlete a unique game plan.
Visit henryford.com/sports or call (313) 972-4216 for an appointment within 24 business hours.
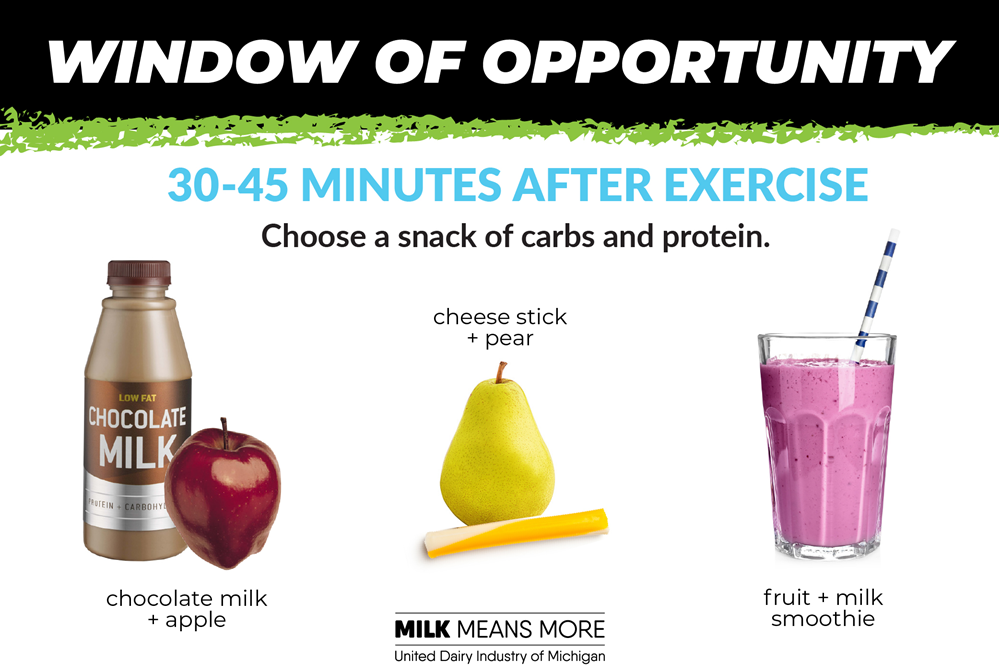
Coach's Guide to Nutrition: Window of Opportunity
May 14, 2024
The 30 minutes following exercise, often referred to as the window of opportunity, is the best time to begin to refuel, rebuild and repair muscles.
 Carbs plus protein in this window can help your students refuel and be ready to attack their next workout.
Carbs plus protein in this window can help your students refuel and be ready to attack their next workout.
After an exercise session or game, muscles are depleted of glycogen, their primary energy source, and are in need of recovery from the stress of training. A small snack is all that is needed in this “window of opportunity.”
The focus should be on carbohydrates with some protein; the ideal snack would have more carbs than protein. Chocolate milk has both carbs and protein, along with electrolytes and fluids to rehydrate. Liquids are also more easily absorbed by the body to help refueling happen more quickly. Other refueling options could include a smoothie, yogurt and granola, or a cheese stick with fruit.
Within 2-3 hours, have a full meal to continue recovery.
Information above is excerpted from UDIM’s A Coach’s Guide to Nutrition.