
Staying Ahead on Head Safety
July 6, 2015
By Rob Kaminski
MHSAA benchmarks editor
Three stacks of concussion-related material offered precious little space on MHSAA Executive Director Jack Roberts’ desk, and perhaps consumed even more room in his head as he tried to wrap his mind around the seemingly daily “latest and greatest” documents outlining signs, detection and return-to-play elements involving head trauma.
Without a doubt, the scene is quite similar on any given day in the offices of his cohorts across the country as school sports leaders are faced with the daunting, dizzying task of devising plans to address concerns aimed at the health of their games.
Lawmakers, rules makers, medical experts and the court of public opinion all want the same thing for student-athletes: a reduction in the chances of head-related injuries. And they all are perfectly willing to offer instant fixes to those in charge.
They often expect those in Roberts’ position to analyze, digest and create action plans as soon as possible without considering the research and resources it will take to get there.
“All parties involved want the same thing. We all want to provide the safest environment for educational athletics through protocols and practices that will offer the most minimal risk of injury,” Roberts said. “But, this can’t be accomplished through unfunded mandates which would stifle the already struggling athletic budgets in many schools.
“Changes have to occur through training and education, orchestrated through state offices and executed locally. And, it takes time to research the best and most effective means. There is so much information, and so many devices in the field today that those in athletic leadership roles almost have to have a medical background as well.”
For instance, there are documents which list as few as five symptoms for concussions, and those listing as many as 15. There are sideline detection methods which purport to take 20 minutes and those which claim to determine concussions in 20 seconds. There are as many return-to-play protocols as there are state associations.
Increasingly, state high school associations are seeking opinions and expertise from local medical personnel. In March, in one of many such meetings, Roberts and other MHSAA staff welcomed several from the Michigan Department of Health and Human Services to their office to discuss sideline detection methods and return-to-play issues.
“There are two areas that concerned us most,” Roberts said. “One, sideline detection of head injuries is inconsistent across the state in terms of both results and resources. Two, we need methods which generate immediate reports and permanent records.”
As the group which convened in March discussed the topic, potential hurdles and new perspectives on sideline management came to the forefront.
On the money and manpower front, who would be responsible for administering sideline tools? Most ideally they would need to be overseen by medical personnel rather than coaches or team managers.
From a perspective standpoint, an interesting view was volleyed out to the group: could sideline detection actually speed up a student’s return to play rather than slow it down? Current protocol prescribes that if competition continues while an athlete is withheld for an apparent concussion, that athlete may not be returned to competition that day but is subject to the return-to-play protocol. And, clearance may not be on the same date on which the athlete was removed from play. Only an M.D., D.O., Physician’s Assistant or Nurse Practitioner may clear the individual to return to activity. With immediate sideline detection, are parties more vulnerable should a student pass immediate tests, only to have undetected effects of the incident increase over time?
“The group shed a different light on the various scenarios, which was a primary purpose for the meeting,” Roberts said. “As one can see, there are so many variables to consider when attempting to determine the next plausible and practical steps toward minimizing and detecting head injuries.
“Further, we have to take into consideration practice sessions as well as competitions, and all sports, not just select sports.”
Adding to the challenge is simply the nature of athletics. Competitors at any level are just that: competitive. Often, students – or their parents – will attempt to hide symptoms or be reluctant to come forward with injuries, particularly head injuries which can’t be seen.
In more cases, perhaps the symptoms simply are not recognized, which is why education is paramount.
First, association leaders have to tackle the due diligence of researching issues and potential solutions to situations currently threatening the well-being of scholastic sports. Considering that some 1,620,000 results are offered when “sideline concussion detection tools” is typed into a search engine, this is a laborious and continual chore.
Such information then needs to be packaged and presented to leaders at the local levels – athletic directors – to pass on to coaches, the individuals who have as much or more influence on students that perhaps any other adults, including parents in some cases.
This is why MHSAA rules meetings, Coaches Advancement Program sessions and other statewide forums continue to bang the drum on health and safety issues; to make sure the messages and procedures reach the student-athletes.
And, it’s why the MHSAA is asking coaches and ADs to be accountable in verifying that the plans in place are being carried out.
Less Could Mean Less
There are times when it’s good to say, “less means more,” but in the case of contact sports, practices and competitions, the idea is for less to mean less. As in less time for collisions to occur yielding fewer injures.
It’s early yet, and one year does not constitute a large sample size, but the MHSAA Football Practice Policy instituted last August could be one step toward reducing head injuries.
Beginning this past football season, the number of practices with helmets, shoulder pads and full pads were limited to start the season, and preseason “collision” sessions were limited to one per day. During the season, such practices were limited to two per week, while the length of practices was also regulated.
Dr. Steven Broglio of the University of Michigan Neurosport department is conducting a three-year study of the Ann Arbor Gabriel Richard football program with the assistance of Richelle Williams to determine the “Effects of Concussion and Sub-Concussion.” The study began in 2013, one year prior to the new MHSAA guidelines.
Research in 2013 showed approximately 650 “impacts” per player. In 2014, the number dropped to approximately 500 impacts per player. Impacts are defined as greater than 10 gs of acceleration. Williams stated that a slap on the back is 4 g, coughing is 3.5 g. On average, a helmet hit is 25-45 g. Concussions usually happen (roughly) between 80-150g.
An encoder is embedded into each football athlete’s helmet which monitors head impacts and exactly where the impact is located. Williams sits at each practice and game and through a pager identifies the player’s number and impact from a hit of 90g or more.
They are also looking at those who do not sustain an impact concussion, but rather sustain multiple head impacts and whether those multiple head impacts lead up to brain changes (measured through EEG).
The initial findings, as submitted by the study team, indicated two reasons why there were fewer overall impacts from 2013 to 2014:
Primary reason: The MHSAA adoption that became effective in August 2014 with new limitations that were placed on “collision practices” and conditions that full pads could not be worn until the fifth day of team practice.
Secondary reason: Fewer players evaluated in 2014 than 2013.
Fit for a King?
Editor’s Note: There are many sideline detection tools on the market, as a quick Google on the topic will reveal. The following, the King-Devick test, is among the highly recommended tests, summarized here simply to provide an idea of the types of systems available and how they operate. The following is from King-Devick’s website.
The King-Devick Test is an objective remove-from-play sideline concussion screening test that can be administered by parents and coaches in minutes. The King-Devick Test is an accurate and reliable method for identifying athletes with head trauma and has particular relevance to: Football, Hockey, Soccer, Basketball, Lacrosse, Rugby, Baseball, Softball and Other Collision Activities.
King-Devick Test is an easy-to-administer test which is given on the sidelines of sporting events to aid in the detection of concussions in athletes. King-Devick Test (K-D Test) can help to objectively determine whether players should be removed from games. As a result, King-Devick Test can help prevent the serious consequences of repetitive concussions resulting from an athlete returning to play after a head injury.
How King-Devick Test Works
Concussions are a complex type of brain injury that is not visible on routine scans of the brain, yet are detectable when important aspects of brain function are measured. King-Devick Test (K-D Test) is a two-minute test that requires an athlete to read single digit numbers displayed on cards or on an iPad. After suspected head trauma, the athlete is given the test and if the time needed to complete the test is any longer than the athlete’s baseline test time, the athlete should be removed from play and should be evaluated by a licensed professional.
Remove-From-Play vs. Return-To-Play
Both remove-from-play and return-to-play decisions are crucial in concussion recovery. It is critical to remove a concussed athlete from play in order to prevent further damage. It is also extremely important to keep the athlete from returning to play until they have made a full recovery. There are tools to assist in making both remove-from-play and return-to-play decisions.
King-Devick Test for Remove-From-Play Decisions
- Quick, objective sideline testing
- Measures impairments of speech, language and other correlates of suboptimal brain function
- Instant screening feedback in minutes
- Administered by parents, coaches, athletic trainers and medical professionals in remove-from-play decisions
- Neurocognitive Testing for Return-To-Play Decisions
- Computerized concussion evaluation system (in the computer lab)
- Measures verbal and visual memory, processing speed and reaction
- Tracks recovery of cognitive processes following concussion
- Assists clinicians in making return-to-play decisions
CPR Training, CAP Add to Preparedness
By
Geoff Kimmerly
MHSAA.com senior editor
October 12, 2015
A recent graduate from Ovid-Elsie High School named Chris Fowler started classes this fall at Michigan State University, his days representing the Marauders on the basketball court, football field and golf course now memories as he starts the next chapter of his young adult life.
But his story also will remain a reminder as his high school’s athletic department prepares each year to keep its athletes as safe as possible.
Three years ago next month, Fowler collapsed on the football practice field in cardiac arrest. The then-sophomore was brought back to life by two of his coaches, who revived him with CPR and an AED machine.
There’s no need for athletic director Soni Latz to recount the events of that day when explaining the importance of being ready to respond to a medical crisis – her coaches are well aware of why Fowler survived and understand completely why they too must be prepared.
“Everyone is very aware of what happened and the importance of being trained and knowing what to do, and actually feeling comfortable to step in and administer CPR when needed,” Latz said. “You can feel it’s never going to happen to you, but once it has, it makes you more aware and conscientious to be prepared.”
But Fowler’s story is worth noting on a larger level as varsity coaches at all MHSAA member schools are required this year for the first time to become certified in CPR, and as the largest classes in Coaches Advancement Program history begin course work that includes up to four modules designed to make them aware of health and safety situations that may arise at their schools as well.
The CPR requirement is the most recent addition to an MHSAA thrust toward raising expectations for coaches’ preparedness. The first action of this effort required all assistant and subvarsity coaches at the high school level to complete the same rules and risk minimization meeting requirement as high school varsity head coaches beginning with the 2014-15 school year.
The next action, following the CPR mandate, will require all persons hired as a high school varsity head coach for the first time at an MHSAA member school after July 31, 2016, to have completed the MHSAA’s Coaches Advancement Program Level 1 or Level 2.
In addition, MHSAA member schools this summer received the “Anyone can Save a Life” program, an emergency action plan curriculum designed by the Minnesota State High School League to help teams – guided by their coaches – create procedures for working together during medical emergencies.
“Coaches get asked to do a lot, and even if a school has an athletic trainer or some other health care professional, that person can’t be everywhere all the time. Coaches often are called upon to be prepared for (medical) situations,” said Gayle Thompson, an adjunct assistant professor at Albion College who formerly directed the athletic training program at Western Michigan University and continues to teach CAP sports medicine modules.
“The more (coaches) can learn to handle the situations that can inevitably arise, the better off they’re going to feel in those situations and the better care they’ll be able to offer their athletes. It’s proven that the faster athletes are able to get care, the quicker they’re able to come back to play.”
 Pontiac Notre Dame Prep – which has sent a number of coaches through the CAP program – began a focus on heart safety about five years ago after a student-athlete was diagnosed with a heart issue that allowed her to continue to play volleyball and softball, but not basketball. Athletic director Betty Wroubel said that prior to the student’s diagnosis, the school did provide training in CPR, AED use and artificial respiration; however, that situation put coaches and administrators further on the alert.
Pontiac Notre Dame Prep – which has sent a number of coaches through the CAP program – began a focus on heart safety about five years ago after a student-athlete was diagnosed with a heart issue that allowed her to continue to play volleyball and softball, but not basketball. Athletic director Betty Wroubel said that prior to the student’s diagnosis, the school did provide training in CPR, AED use and artificial respiration; however, that situation put coaches and administrators further on the alert.
Her school offers CPR training also to subvarsity and middle school coaches, using a combination of video instruction from the American Red Cross and in-person guidance by members of the school community who are certified to teach those skills. Students at the school also have received training – and it paid off a few years ago when one of them gave CPR to a baby who had stopped breathing at a local shopping mall.
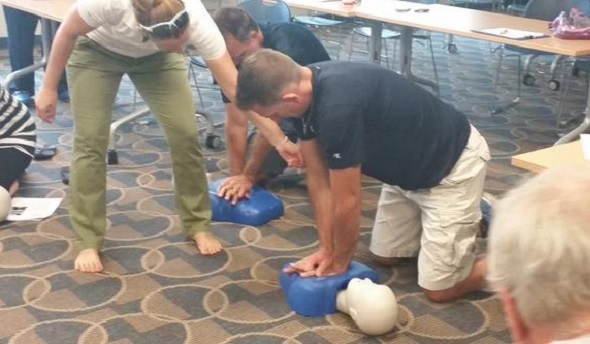
Portage Central scheduled two sessions this fall for its coaches to receive not only CPR certification, but AED training as well. Central was fortunate to have an American Red Cross first-aid trainer in house, teacher Rachel Flachs, who also is close to the athletic side as the girls swimming and diving coach at Mattawan High School.
Central athletic director Joe Wallace said the training was offered not just to varsity head coaches, but every head coach on every level of the program so that “at least we know that at every given practice, every game, we’d have someone recently trained,” he said.
And he was proud of how his coaches immersed themselves in the subject matter.
“They were putting themselves in scenarios to see how it related to their own sports and asking really great questions,” Wallace said. “It was thought provoking.”
The CAP sports medicine modules are designed to do the same as coaches consider the medical situations they could face. They aren’t designed as “medical training,” said Tony Moreno, a professor of kinesiology at Eastern Michigan University and teacher of all four CAP sports medicine modules. Rather, attendees receive an awareness and basic education on common injuries, injury mechanisms and prevention, and how to create an action plan in the event of an injury incident.
The CAP program touches on a variety of safety topics in several of the available seven levels of coach education.
CAP 1 – which is part of the mandate for new coaches beginning next school year – includes “Sports Medicine and First Aid.” Cap 4 has modules titled “Understanding Athlete Development” and “Strength and Conditioning: Designing Your Program.” CAP 5 includes the session, “Peak Health and Performance.” Attendees also have the option of receiving CPR and AED training as an addition to some courses.
With a quick Internet search, coaches have no trouble finding a variety of resources on sports medicine, performance enhancement, nutrition and healthy living regarding young athletes. “However, some of these sources are more credible and scientifically-based in comparison to others,” Moreno said. “CAP strives on an annual basis to continue to update and improve the quality and credibility of this information and in a face-to-face manner where coaches have the opportunity to ask questions about their experiences and specific programs.”
“Having the CAP requirement will only make them better informed. Many have had this kind of information before, but there’s always something new coming,” Thompson added. “I think we do a good job, not of trying to tell them they were wrong, but maybe taking what they’ve known a step further and making them better prepared – empowering them to do their best.”
Wroubel may understand more than most athletic directors the growing list of tasks coaches are asked to accomplish; she’s also one of the winningest volleyball and softball coaches in MHSAA history and continues to guide both Fighting Irish programs.
But she and Wallace both said the CPR mandate isn’t considered another box to check on a to-do list; there’s enthusiasm because of its importance and the opportunity to carry those skills into other areas of community life as well.
Wroubel has served as a coach since 1975 and said this renewed emphasis on coaches having knowledge of sports medicine actually is a return to how things were when she started. Back then, coaches were responsible for being that first line of medical know-how, from taping ankles to providing ice and evaluating when their athletes should make a trip to the doctor’s office.
“When I first started coaching, we didn’t have sports medicine people, trainers, or team doctors other than for football. You did everything yourself,” Wroubel said. “I think everybody got away from that, but I think it’s coming back because a trainer can’t be everywhere.
“It’s healthy and it’s good for kids. … The more of us with emergency skills, the better we’re able to serve our community.”
PHOTOS: (Top) Portage Central coaches receive CPR training earlier this fall. (Middle) Pontiac Notre Dame Prep coaches practice during AED training. (Photos courtesy of school athletic departments.)

