CPR Training, CAP Add to Preparedness
By
Geoff Kimmerly
MHSAA.com senior editor
October 12, 2015
A recent graduate from Ovid-Elsie High School named Chris Fowler started classes this fall at Michigan State University, his days representing the Marauders on the basketball court, football field and golf course now memories as he starts the next chapter of his young adult life.
But his story also will remain a reminder as his high school’s athletic department prepares each year to keep its athletes as safe as possible.
Three years ago next month, Fowler collapsed on the football practice field in cardiac arrest. The then-sophomore was brought back to life by two of his coaches, who revived him with CPR and an AED machine.
There’s no need for athletic director Soni Latz to recount the events of that day when explaining the importance of being ready to respond to a medical crisis – her coaches are well aware of why Fowler survived and understand completely why they too must be prepared.
“Everyone is very aware of what happened and the importance of being trained and knowing what to do, and actually feeling comfortable to step in and administer CPR when needed,” Latz said. “You can feel it’s never going to happen to you, but once it has, it makes you more aware and conscientious to be prepared.”
But Fowler’s story is worth noting on a larger level as varsity coaches at all MHSAA member schools are required this year for the first time to become certified in CPR, and as the largest classes in Coaches Advancement Program history begin course work that includes up to four modules designed to make them aware of health and safety situations that may arise at their schools as well.
The CPR requirement is the most recent addition to an MHSAA thrust toward raising expectations for coaches’ preparedness. The first action of this effort required all assistant and subvarsity coaches at the high school level to complete the same rules and risk minimization meeting requirement as high school varsity head coaches beginning with the 2014-15 school year.
The next action, following the CPR mandate, will require all persons hired as a high school varsity head coach for the first time at an MHSAA member school after July 31, 2016, to have completed the MHSAA’s Coaches Advancement Program Level 1 or Level 2.
In addition, MHSAA member schools this summer received the “Anyone can Save a Life” program, an emergency action plan curriculum designed by the Minnesota State High School League to help teams – guided by their coaches – create procedures for working together during medical emergencies.
“Coaches get asked to do a lot, and even if a school has an athletic trainer or some other health care professional, that person can’t be everywhere all the time. Coaches often are called upon to be prepared for (medical) situations,” said Gayle Thompson, an adjunct assistant professor at Albion College who formerly directed the athletic training program at Western Michigan University and continues to teach CAP sports medicine modules.
“The more (coaches) can learn to handle the situations that can inevitably arise, the better off they’re going to feel in those situations and the better care they’ll be able to offer their athletes. It’s proven that the faster athletes are able to get care, the quicker they’re able to come back to play.”
 Pontiac Notre Dame Prep – which has sent a number of coaches through the CAP program – began a focus on heart safety about five years ago after a student-athlete was diagnosed with a heart issue that allowed her to continue to play volleyball and softball, but not basketball. Athletic director Betty Wroubel said that prior to the student’s diagnosis, the school did provide training in CPR, AED use and artificial respiration; however, that situation put coaches and administrators further on the alert.
Pontiac Notre Dame Prep – which has sent a number of coaches through the CAP program – began a focus on heart safety about five years ago after a student-athlete was diagnosed with a heart issue that allowed her to continue to play volleyball and softball, but not basketball. Athletic director Betty Wroubel said that prior to the student’s diagnosis, the school did provide training in CPR, AED use and artificial respiration; however, that situation put coaches and administrators further on the alert.
Her school offers CPR training also to subvarsity and middle school coaches, using a combination of video instruction from the American Red Cross and in-person guidance by members of the school community who are certified to teach those skills. Students at the school also have received training – and it paid off a few years ago when one of them gave CPR to a baby who had stopped breathing at a local shopping mall.
Portage Central scheduled two sessions this fall for its coaches to receive not only CPR certification, but AED training as well. Central was fortunate to have an American Red Cross first-aid trainer in house, teacher Rachel Flachs, who also is close to the athletic side as the girls swimming and diving coach at Mattawan High School.
Central athletic director Joe Wallace said the training was offered not just to varsity head coaches, but every head coach on every level of the program so that “at least we know that at every given practice, every game, we’d have someone recently trained,” he said.
And he was proud of how his coaches immersed themselves in the subject matter.
“They were putting themselves in scenarios to see how it related to their own sports and asking really great questions,” Wallace said. “It was thought provoking.”
The CAP sports medicine modules are designed to do the same as coaches consider the medical situations they could face. They aren’t designed as “medical training,” said Tony Moreno, a professor of kinesiology at Eastern Michigan University and teacher of all four CAP sports medicine modules. Rather, attendees receive an awareness and basic education on common injuries, injury mechanisms and prevention, and how to create an action plan in the event of an injury incident.
The CAP program touches on a variety of safety topics in several of the available seven levels of coach education.
CAP 1 – which is part of the mandate for new coaches beginning next school year – includes “Sports Medicine and First Aid.” Cap 4 has modules titled “Understanding Athlete Development” and “Strength and Conditioning: Designing Your Program.” CAP 5 includes the session, “Peak Health and Performance.” Attendees also have the option of receiving CPR and AED training as an addition to some courses.
With a quick Internet search, coaches have no trouble finding a variety of resources on sports medicine, performance enhancement, nutrition and healthy living regarding young athletes. “However, some of these sources are more credible and scientifically-based in comparison to others,” Moreno said. “CAP strives on an annual basis to continue to update and improve the quality and credibility of this information and in a face-to-face manner where coaches have the opportunity to ask questions about their experiences and specific programs.”
“Having the CAP requirement will only make them better informed. Many have had this kind of information before, but there’s always something new coming,” Thompson added. “I think we do a good job, not of trying to tell them they were wrong, but maybe taking what they’ve known a step further and making them better prepared – empowering them to do their best.”
Wroubel may understand more than most athletic directors the growing list of tasks coaches are asked to accomplish; she’s also one of the winningest volleyball and softball coaches in MHSAA history and continues to guide both Fighting Irish programs.
But she and Wallace both said the CPR mandate isn’t considered another box to check on a to-do list; there’s enthusiasm because of its importance and the opportunity to carry those skills into other areas of community life as well.
Wroubel has served as a coach since 1975 and said this renewed emphasis on coaches having knowledge of sports medicine actually is a return to how things were when she started. Back then, coaches were responsible for being that first line of medical know-how, from taping ankles to providing ice and evaluating when their athletes should make a trip to the doctor’s office.
“When I first started coaching, we didn’t have sports medicine people, trainers, or team doctors other than for football. You did everything yourself,” Wroubel said. “I think everybody got away from that, but I think it’s coming back because a trainer can’t be everywhere.
“It’s healthy and it’s good for kids. … The more of us with emergency skills, the better we’re able to serve our community.”
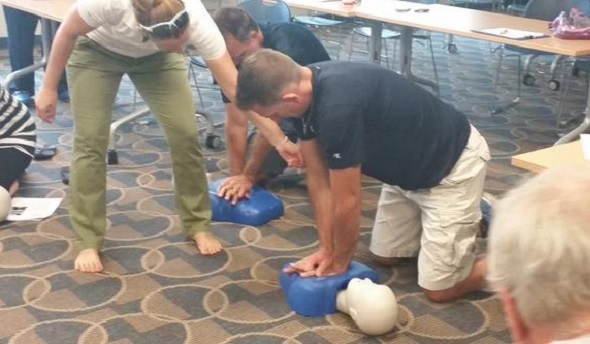
PHOTOS: (Top) Portage Central coaches receive CPR training earlier this fall. (Middle) Pontiac Notre Dame Prep coaches practice during AED training. (Photos courtesy of school athletic departments.)

Health & Safety: A Look Back, Gallop Ahead
By
John E. (Jack) Roberts
MHSAA Executive Director, 1986-2018
August 7, 2015
By Jack Roberts
MHSAA executive director
We are just completing year six of eight during which we have been addressing the four important health and safety issues that, for ease of conversation, we call the “Four Hs.”
During the 2009-10 and 2010-11 school years, our focus was on Health Histories. We made enhancements in the pre-participation physical examination form, stressing the student’s health history, which we believe was and is the essential first step to participant health and safety.
During the 2011-12 and 2012-13 school years, our focus was on Heads. We were an early adopter of removal-from-play and return-to-play protocols, and our preseason rules/risk management meetings for coaches included information on concussion prevention, recognition and aftercare.
Without leaving that behind, during the 2013-14 and 2014-15 school years, our focus was on Heat – acclimatization. We adopted a policy to manage heat and humidity – it is recommended for regular season and it’s a requirement for MHSAA tournaments. The rules/risk management meetings for coaches during these years focused on heat and humidity management.
At the mid-point of this two-year period, the MHSAA adopted policies to enhance acclimatization at early season practices and to reduce head contact at football practices all season long.
Without leaving any of the three previous health and safety “H’s” behind, during the 2015-16 and 2016-17 school years, our focus will be on Hearts – sudden cardiac arrest and sudden cardiac death.
Coinciding with this emphasis is the requirement that all high school level, varsity level head coaches be CPR certified starting this fall. Our emphasis will be on AEDs and emergency action plans – having them and rehearsing them.
On Feb. 10, bills were introduced into both the U.S. Senate and House of Representatives, together called the “Safe Play Act (see below),” which addressed three of the four health and safety “H’s” just described: Heat, Hearts and Heads.
For each of these topics, the federal legislation would mandate that the director of the Centers for Disease Control develop educational material and that each state disseminate that material.
For the heat and humidity management topic, the legislation states that schools will be required to adopt policies very much like the “MHSAA Model Policy to Manage Heat and Humidity” which the MHSAA adopted in March of 2013.
For both the heart and heat topics, schools will be required to have and to practice emergency action plans like we have been promoting in the past and distributed to schools this summer.
For the head section, the legislation would amend Title IX of the 1972 Education Amendments and eliminate federal funding to states and schools which fail to educate their constituents or fail to support students who are recovering from concussions. This support would require multi-disciplinary concussion management teams that would include medical personnel, parents and others to provide academic accommodations for students recovering from concussions that are similar to the accommodations that are already required of schools for students with disabilities or handicaps.
This legislation would require return-to-play protocols similar to what we have in Michigan, and the legislation would also require reporting and recordkeeping that is beyond what occurs in most places.
This proposed federal legislation demonstrates two things. First, that we have been on target in Michigan with our four Hs – it’s like they read our playbook of priorities before drafting this federal legislation.
This proposed federal legislation also demonstrates that we still have some work to do.
And what will the following two years – 2017-18 and 2018-19 – bring? Here are some aspirations – some predictions, but not quite promises – of where we will be.
First, we will have circled back to the first “H” – Health Histories – and be well on our way to universal use of paperless pre-participation physical examination forms and records.
Second, we will have made the immediate reporting and permanent recordkeeping of all head injury events routine business in Michigan school sports, for both practices and contests, in all sports and at all levels.
Third, we will have added objectivity and backbone to removal from play decisions for suspected concussions at both practices and events where medical personnel are not present; and we could be a part of pioneering “telemedicine” technology to make trained medical personnel available at every venue for every sport where it is missing today.
Fourth, we will have provided a safety net for families who are unable to afford no-deductible, no exclusion concussion care insurance that insists upon and pays for complete recovery from head injury symptoms before return to activity is permitted.
We should be able to do this, and more, without judicial threat or legislative mandate. We won’t wait for others to set the standards or appropriate the funds, but be there to welcome the requirements and resources when they finally arrive.
Safe Play Act — H.R.829
114th Congress (2015-2016) Introduced in House (02/10/2015)
Supporting Athletes, Families and Educators to Protect the Lives of Athletic Youth Act or the SAFE PLAY Act
Amends the Public Health Service Act to require the Centers for Disease Control and Prevention (CDC) to develop public education and awareness materials and resources concerning cardiac health, including:
- information to increase education and awareness of high risk cardiac conditions and genetic heart rhythm abnormalities that may cause sudden cardiac arrest in children, adolescents, and young adults;
- sudden cardiac arrest and cardiomyopathy risk assessment worksheets to increase awareness of warning signs of, and increase the likelihood of early detection and treatment of, life-threatening cardiac conditions;
- training materials for emergency interventions and use of life-saving emergency equipment; and
- recommendations for how schools, childcare centers, and local youth athletic organizations can develop and implement cardiac emergency response plans.
Requires the CDC to: (1) provide for dissemination of such information to school personnel, coaches, and families; and (2) develop data collection methods to determine the degree to which such persons have an understanding of cardiac issues.
Directs the Department of Health and Human Services to award grants to enable eligible local educational agencies (LEAs) and schools served by such LEAs to purchase AEDs and implement nationally recognized CPR and AED training courses.
Amends the Elementary and Secondary Education Act of 1965 to require a state, as a condition of receiving funds under such Act, to certify that it requires: (1) LEAs to implement a standard plan for concussion safety and management for public schools; (2) public schools to post information on the symptoms of, the risks posed by, and the actions a student should take in response to, a concussion; (3) public school personnel who suspect a student has sustained a concussion in a school-sponsored activity to notify the parents and prohibit the student from participating in such activity until they receive a written release from a health care professional; and (4) a public school's concussion management team to ensure that a student who has sustained a concussion is receiving appropriate academic supports.
Directs the National Oceanic and Atmospheric Administration to develop public education and awareness materials and resources to be disseminated to schools regarding risks from exposure to excessive heat and humidity and recommendations for how to avoid heat-related illness. Requires public schools to develop excessive heat action plans for school-sponsored athletic activities.
Requires the CDC to develop guidelines for the development of emergency action plans for youth athletics.
Authorizes the Food and Drug Administration to develop information about the ingredients used in energy drinks and their potential side effects, and recommend guidelines for the safe use of such drinks by youth, for dissemination to public schools.
Requires the CDC to: (1) expand, intensify, and coordinate its activities regarding cardiac conditions, concussions, and heat-related illnesses among youth athletes; and (2) report on fatalities and catastrophic injuries among youths participating in athletic activities.

